280 Australians develop diabetes every day, which can lead to heart disease, kidney disease, erectile dysfunction, vision impairment, amputation, requirement for medications and poor quality of life.
“Type 2 diabetes is the world’s fastest growing medical condition and the greatest public health crisis of our time.”
Dr Michael Mosley.
At MHS, we are passionate about helping people make an informed decision about their health and specialise in complex obesity, such as those with diabetes. We understand that the diagnosis of diabetes itself, and the plethora of information available can be overwhelming, so the following blog aims to cover the latest updates/research in the area of diabetes and remission to reduce the confusion and optimise outcomes. It also features the opinions of leading experts to answer these important questions.
Is diabetes remission possible and for whom?
Why should it be considered?
What approaches may be most effective?
“Patients who develop type 2 diabetes, until earlier this year they were told this is a progressive disease, you’re most likely to need medication and insulin…But it is not, it doesn’t have to be. There is the opportunity to put type 2 diabetes into remission.”
Dr James Muecke, Eye surgeon and Australian of the Year 2020.
How does type 2 diabetes (T2D) develop?
Although the exact cause of T2D is unknown, it’s strong link to obesity and excess fat has prompted researchers to explore the role of fat burning (Pujia et al., 2019) and contributing factors such as lifestyle. It is likely to occur when an individual’s Personal Fat Threshold (PFT) is exceeded, leading to fat spill-over into the liver and pancreas (Mrabeh A, 2020). Having a low PFT (possibly genetic) might explain why someone can be thin yet develop T2D, while someone obese might not.
“It was incredible. I looked into it and had an epiphany. I realised I had been failing my patients for years by swallowing the conventional wisdom that we have to medicate our way out of this chronic illness without stopping to think about its actual cause.”
Dr David Unwin, UK GP who has helped more than 100 patients put their diabetes into remission.
If we can measure and find ways to increase our fat burning, diabetes remission just may be possible.
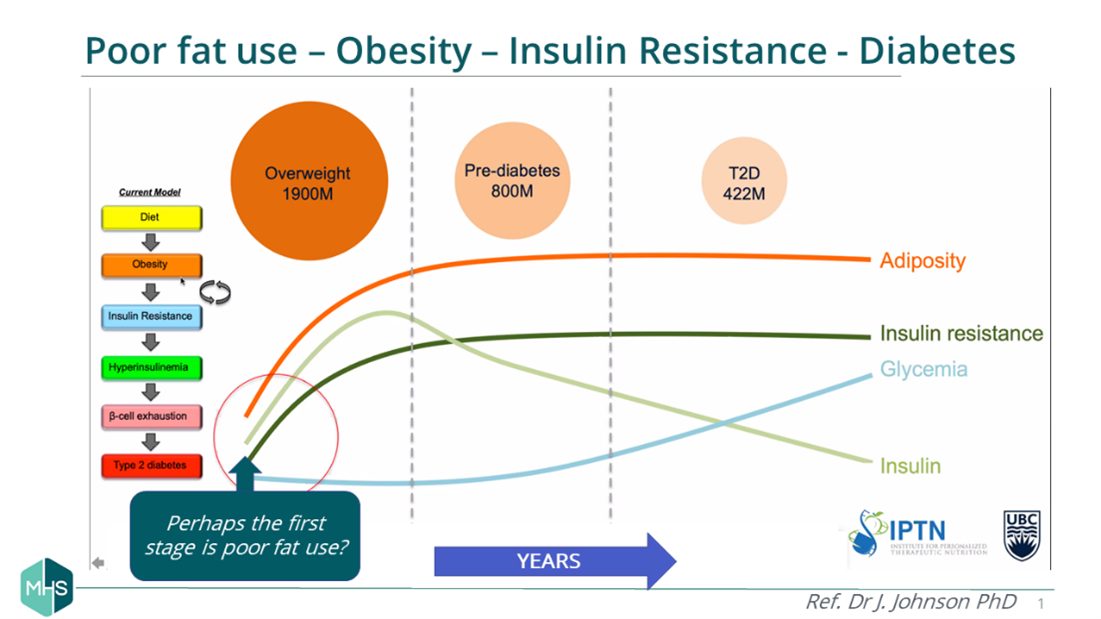
Proposed time course of T2D
Is remission possible?
The diagnosis of a chronic, progressive condition can sometimes feel like a unremovable curse. If you progressively worsen and can’t avoid complications and premature death, then why struggle with your diet and managing your diabetes? But views are changing….
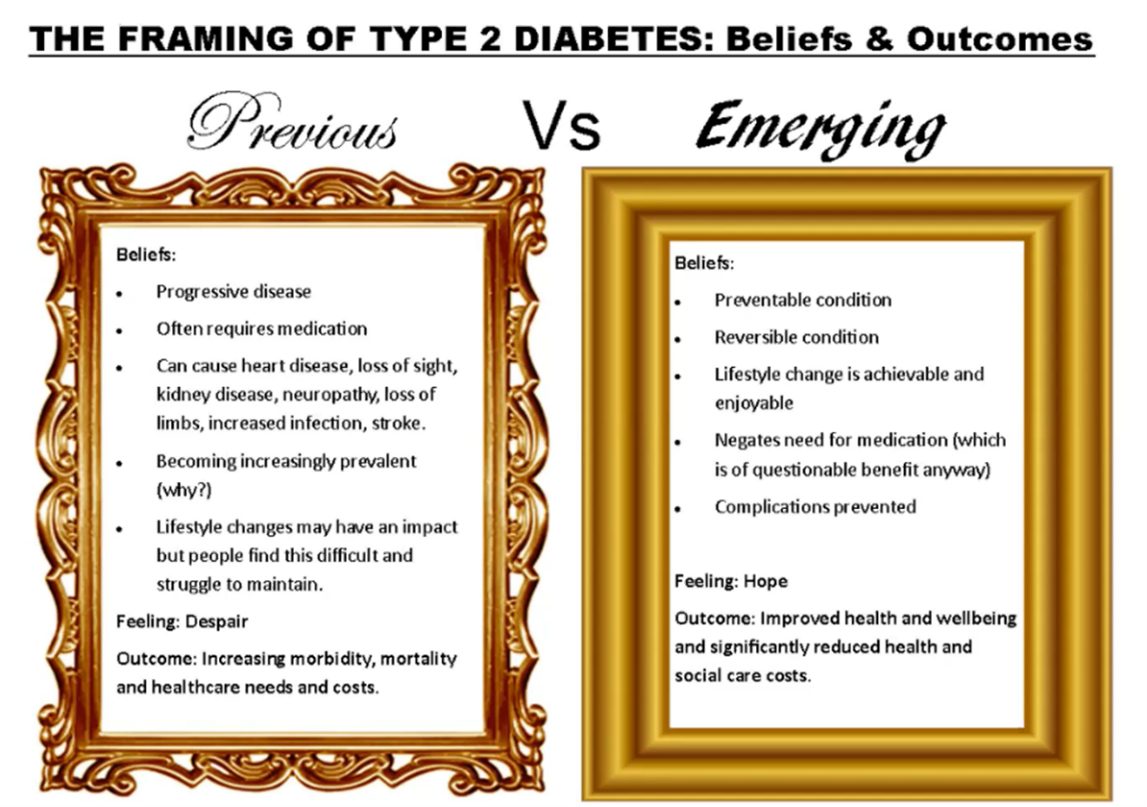
Used with permission: Dr Campbell Murdoch, UK GP
Research now recognised by Diabetes Australia, shows that it is possible for some people with T2D to achieve remission - defined as an HbA1c of under 6.5% for at least three months without the need for glucose lowering medications (Diabetes Australia, 2021). Diabetes WA also recognise this, but their recent survey showed there is uncertainty. Many felt remission would give them a feeling of hope and would try it, but some health professionals did not consider it possible or were unsure.
“It’s not a question of whether remission of T2 diabetes can occur. The research has shown that constantly. The question is how many can achieve it? The research shows that remission is possible for between 20%-75% of those with T2D if weight loss is achieved early enough. But even at 20% that would be over 200,000 Aussies, never mind the amount that would reduce medications.”
Ray Kelly, AEP. PhD Candidate and Founder of the Too Deadly for Diabetes Aboriginal Healthcare program.
The pursuit of remission can reduce the need for medication, dramatically improve energy levels, lead to better weight management and should prevent long term complications such as neuropathy (nerve damage), amputation and vision impairment. Not only should this reduce healthcare costs, it improves the quality of life for people with diabetes and their families.
What approaches may be most effective?
Exercise, sleep and stress all play a role in metabolic health and T2D management, however diet is key, and without appropriate change other strategies are likely to be ineffective.
“Lifestyle and dietary intervention remain the pinnacle of treatment of chronic disease. New research reaffirming that healthy weight loss can be associated be a reduction in medications and improvement in overall quality of life.”
Dr Ben Ng, Founder of Arden Endocrinology, Singapore.
Addressing unhealthy body fat is a key step to improving glucose control but you want that to be approached in a healthy and sustainable way. MHS provide a personalised approach to help you protect muscle whilst losing body fat. This metabolic approach can help to minimise hunger, manage central obesity and reduce the need for medications.
So let’s explore the options….
1) Very Low Calorie Diets
Traditionally, calorie restriction (typically using shakes and/or non-starchy vegetables) has been shown to be effective for T2D remission. This approach is suitable for someone who is metabolically flexible (able to burn fat – assessed with metabolism testing), and also where fasting protocols may be applicable.
- Rapid improvements in HbA1c and weight
- No surgical risk
- Rebound in both weight and HbA1c
- Hunger and fatigue
- Metabolic decline
- One study showed that an 8 week, 800 kcal per day diet was able to achieve remission from diabetes in 7 of the 11 participants that took part. The trial used MRI scans and showed that the reversal of diabetes appeared to be correlated with significant reductions in fat storage within the liver and pancreas (Lim et al., 2011)
- 1/3 participants with T2D sustained remission for 24 months using a similar diet to that above, followed by a lower calorie weight maintenance diet (Lean et al., 2019)
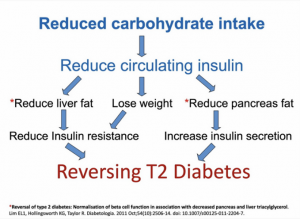
2) Low Carbohydrate Diets
Low-carbohydrate diets are known for lowering the amount of insulin the body needs to produce, resulting in better blood sugar control, less insulin resistance, and improvements in associated symptoms.
- Sustainable
- No surgical risk
- Reduced hunger
- Safe (no hypoglycaemia – Virta)
- No special foods (like shakes)
- Requires long term adherence
- Choices can be difficult in today’s food environment
- Cultural, ethical, and emotional ties to food (religion, vegan, addiction)
- High levels of support may be required
- Multiple approaches for developing and delivering a low-carbohydrate diet intervention for T2D management are safe and effective (Turton et al., 2019)
- After 6 months, the low-carb group had a lower average HbA1c level and had lost more weight than the low-calorie group, and 95% were able to reduce or totally eliminate their diabetes medicines (Westman et al., 2008)
- A low-carbohydrate Mediterranean diet was able to achieve significant rates of remission in people with type 2 diabetes. After one year of following the diet, 15% of participants achieved remission compared to only 4% on the low fat diet (Diabetes Co UK, 2014)
“If you cut out the carbohydrates, your blood sugar goes down, and you lose weight, which lowers your blood sugar even further. It’s a one-two punch.”
Dr Eric Westman, director of Duke University Lifestyle Medicine Program.
Find out how much sugar is hiding in your food - click here.
3) Bariatric Surgery
Weight loss surgery, also known as bariatric surgery, changes the anatomy of the stomach and intestines and makes it harder to eat and digest large quantities of food. Although surgery is drastic, this intervention has shown significant results in reversing type 2 diabetes, with gastric bypass surgery leading the way with the most impressive results, but also coming with the highest risk.
- Largest evidence base
- It works, and quickly
- Involves surgery (and associated complications)
- Weight regain - for long term success lifestyle changes must still be addressed.
- Micronutrient deficiency
- Cost
- 24% of participants with type 2 achieved remission six years after receiving gastric bypass surgery (Brethauer et al., 2013)
- Weight regain is observed within 24 months after surgery in approximately 50% of patients (Magro et al., 2008)
Glucose improvements can occur even before significant weight loss is achieved. Some experts believe this is because the surgery affects gut hormones, which may impact pancreatic function.
How can MHS help?
 MHS are the only clinical service that routinely measures metabolism and uses this information to personalise a weight and fat loss program. Our programs have helped over 1,200 Western Australians and are designed to help you;
MHS are the only clinical service that routinely measures metabolism and uses this information to personalise a weight and fat loss program. Our programs have helped over 1,200 Western Australians and are designed to help you;
- Explore your options
- Learn to burn fat and protect muscle
- Lose weight without hunger
- Reduce medications
- Regain your quality of life
Here is an example of the kind of program and success we can achieve with diabetes.
MHS T2D remission action plan
Before embarking on your own journey, it’s important to talk to your GP about lifestyle changes so that your medications are adjusted safely with blood sugar improvement. Our experience is that most GPs are happy that you are considering weight loss and will support your choice, however as the Diabetes WA survey suggested, some may not be familiar with T2D remission and we can work with them to help you.
Our program includes baseline and progressive testing and the necessary nutrition and exercise programs personalised to your metabolic results. Testing can include:
- Metabolic Testing
- Body Composition Testing
- Metabolic Pathology
For a more detailed breakdown of the MHS metabolic weight management program please click here.
"Being overweight has been a life-long battle, Kirsty has shown me that with science I can have remarkable results...i am feeling fitter than I have in years and looking forward to actively living longer. Thank You”
F, 61, foster mum.
“I love that the program is personalised to the individual and I highly recommend for those wanting to get their health back!”
F, 37.
Summary
 In a nutshell, T2D remission is possible, particularly when physiology is addressed to improve metabolic health and achieve substantial and sustainable fat loss! Everyone’s journey is different, so while the achievement of defined remission standards may not happen for everyone, our T2D patients and others world-wide have achieved significant health gains.
In a nutshell, T2D remission is possible, particularly when physiology is addressed to improve metabolic health and achieve substantial and sustainable fat loss! Everyone’s journey is different, so while the achievement of defined remission standards may not happen for everyone, our T2D patients and others world-wide have achieved significant health gains.
It’s wonderful news that people with T2D now have a recognised option to pursue remission. If this blog has helped you to understand about that topic, the role of metabolism, and how you might achieve better T2D health, please share far and wide. Thank you!
Note: This blog is not intended to be a substitute for professional medical advice. Please consult with your GP regarding diabetes remission and changes in your medication.
